NIH Fails to Institute Health
war-on-disease, 1-percent-treaty, medical-research, public-health, peace-dividend, decentralized-trials, dfda, dih, victory-bonds, health-economics, cost-benefit-analysis, clinical-trials, drug-development, regulatory-reform, military-spending, peace-economics, decentralized-governance, wishocracy, blockchain-governance, impact-investing
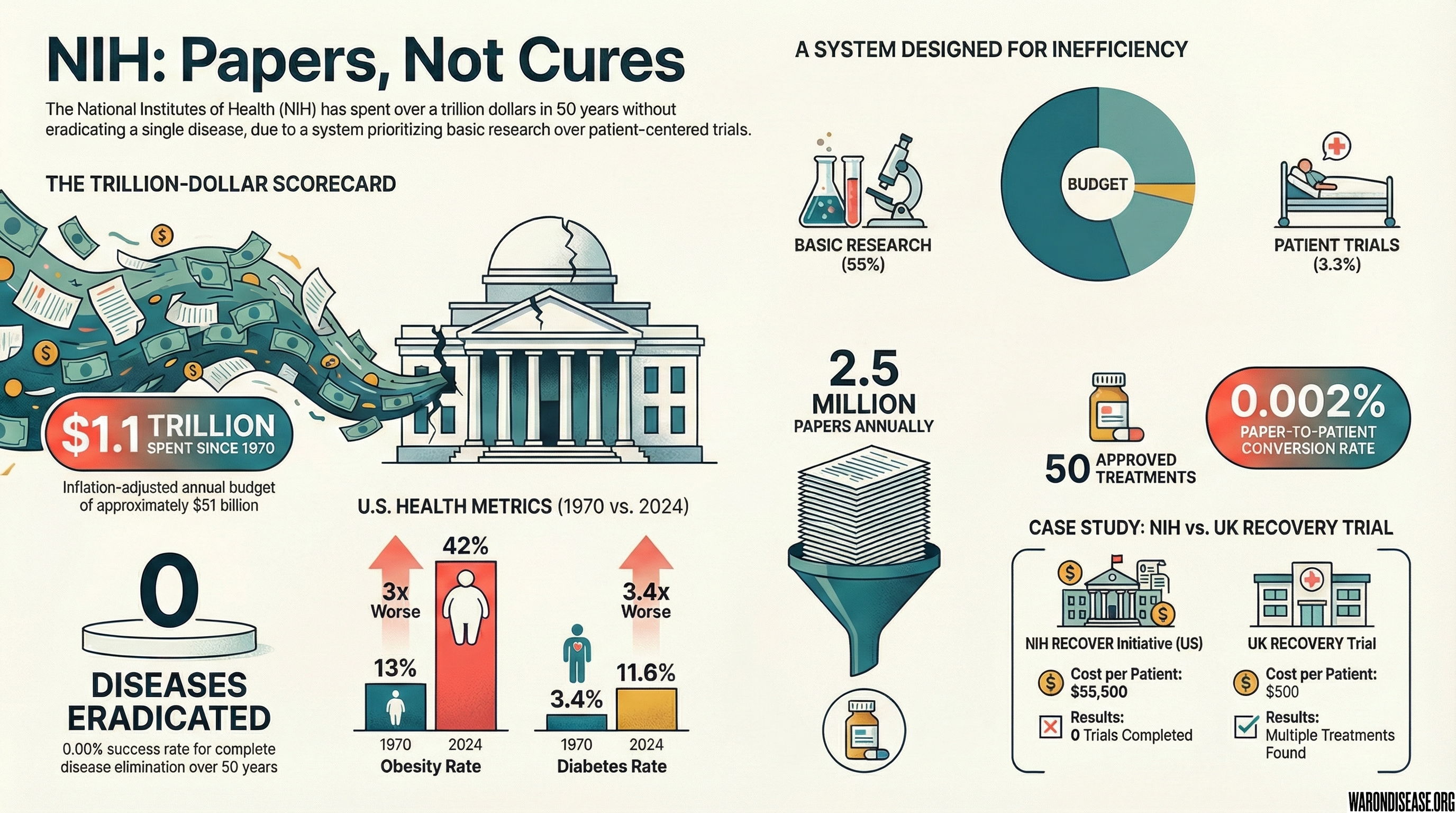
With an annual budget of approximately $51 billion, the National Institutes of Health has spent over $1.1 trillion since 1970 (inflation-adjusted).
Number of diseases the NIH has eradicated: Zero.
Success rate: 0.00% for complete disease elimination.
A medical politburo in Maryland deciding which of 10,000 diseases matter. Yours doesn’t.
They fund what gets published, not what saves lives.
Result: 55 million die annually while papers get published.
To be fair, eradicating disease is hard. Just ask the WHO, who eradicated smallpox for $300 million (smallpox was WHO, not NIH). Or ask Jonas Salk, who developed the polio vaccine in a university lab. Or ask the veterinarians, who’ve eradicated multiple animal diseases while the NIH was forming subcommittees.
The Translation Crisis: Concept Rich, Trial Poor
Here is the “Stock vs Flow” problem in one sentence: We are not short of hypotheses; we are short of trial slots.
- FDA-approved drugs: >20,000 known safe in humans
- Repurposable compounds: ~4,700-6,800 clinically-tested candidates (including 3,422 marketed drugs) sitting on shelves
- Plausible dementia interventions: Hundreds
- Clinical trials available for your grandma in St. Louis: Zero
We have a massive stock of safe molecules that have never been systematically evaluated for new uses. But the flow of trials is a trickle.
The $600,000 Meta-Research Masterpiece
After searching clinicaltrials.gov for dementia trials your grandma could join, one finally appears.
It’s a study asking if people would be interested in dementia trials.
- Cost: $600,000
- Purpose: Survey research about hypothetical willingness to participate
- Patients treated: Zero
- Treatments tested: Zero
Let’s be clear: This isn’t the researcher’s fault. They wrote the grant NIH rewards. They’re playing the game correctly.
The problem is the game itself.
NIH will fund $600,000 to ask if people want trials. But it won’t fund the actual trials people want to join.
We already know the answer: ~50-75% of patients say they’re willing to participate, but only ~10% are ever invited.
The bottleneck isn’t information about willingness. It’s capacity.
That $600,000 could have funded: - 1,200 Alzheimer’s patients in pragmatic trials (at $500/patient, UK RECOVERY model) - Testing 5-10 repurposed drugs we already know are safe - Actual data on whether treatments work
Instead, we got confirmation that people dying of dementia would like not to die of dementia.
This is what happens when the system rewards papers about trials more than running trials.
The Basic Research Black Hole
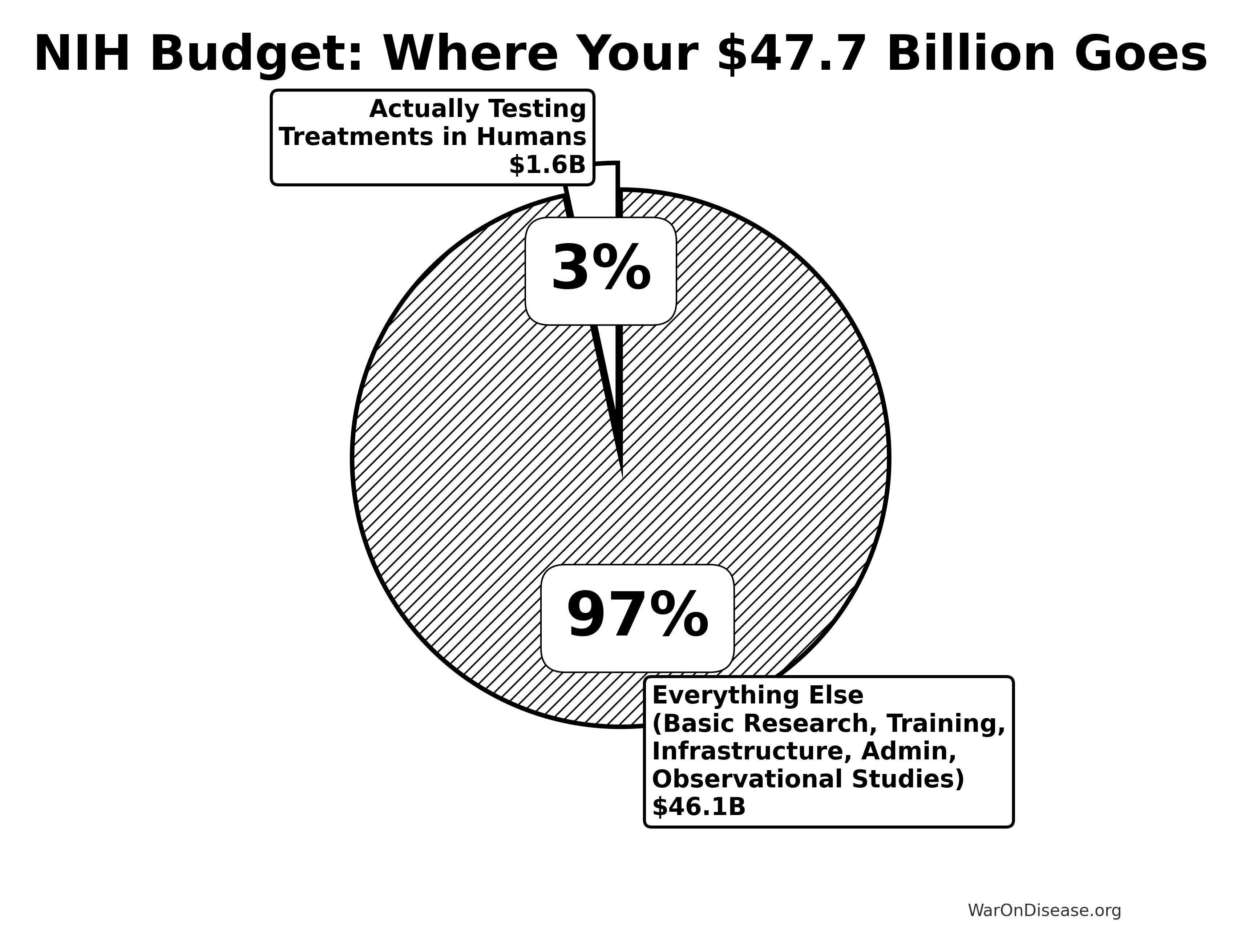
The NIH spend the vast majority of it on “basic research”, understanding disease in mice, while a tiny fraction goes to testing treatments in actual humans.
The Allocation Disaster
Here’s where the FY2017-2021 budget actually goes:
- Basic research (mice and molecules): 72% ($97B)
- “Clinical trials and related activities”: 21% ($28B)
- Training programs: 7% ($9B)
But here’s the scam: that “21% for clinical trials” sounds impressive until you see what it actually includes:
- Actual drug treatment trials (Phases 1-3): Only 3.3% of total budget ($8.1B over 2010-2019)
- Phase 3 trials (where treatments are proven effective): NIH covers only 3.7-4.3% of costs, abandoning funding at the critical stage
- Pragmatic trials (30x cheaper than traditional trials): Severely underfunded despite massive cost advantage
- Observational studies: Watching you get sicker (All of Us - $2.16B, zero treatments tested)
- Infrastructure programs: CTSA network buildings and overhead, not treating patients
- Health services research, epidemiology, behavioral studies: The remaining 17.7% that sounds like “clinical research”
The result is a system that produces papers, not cures:
- Papers published: 2.5 million annually
- New treatments approved: ~50 annually
- Conversion rate from paper to patient: 0.002%
Knowledge Production: Saturated. Translation Capacity: Starved.
The bottleneck isn’t ideas. It’s execution:
- Biomedical papers produced: 2.5 million per year
- Adults who’ve participated in trials: ~5%
- Adults willing to participate if invited: ~50-75%
- Adults actually invited: ~9-11%
We’re drowning in hypotheses while patients are starving for trial slots.
The system produces millions of papers testing ideas in mice, but offers trial participation to only 5% of humans. Even though half would say yes if asked.
That’s not an information failure. That’s a capacity failure.
We know everything about how cancer works in mice. We’ve mapped every pathway, gene, and protein. We have Nobel Prizes for understanding mechanisms.
What we don’t have: Cures.
Because understanding disease and curing disease are completely different things. The NIH chose understanding. Patients needed cures.
The Public Goods vs. Club Goods Scam
The NIH defends its existence by claiming to produce “Public Goods” (open science, data, training). In reality, it spends taxpayers’ money to produce “Club Goods” for private industry.
The Scam in Numbers:
- Direct commercialization support: ~3-5% of budget
- Indirect subsidy to profitable firms: ~40-60% of NIH spending functions as a de facto subsidy to industry. This includes funding basic research, training scientists, and generating patents that private companies exploit
- NIH contribution to approved drugs: Funded research for 99% of new drugs (356 drugs, 2010-2019), but covers only ~10% of clinical trial costs
- Who pays for translation: NIH covers only ~10% of what industry spends on clinical trials for approved drugs
The pattern is clear: taxpayers fund 40-60% of the knowledge pipeline (~$20-30B/year), industry patents the winners, and the public pays again through high drug prices.
When a discovery leads to a blockbuster drug, the IP is privatized. When the research leads to a dead end, the public eats the loss.
Socialized Risk, Privatized Profit.
True public goods would be unpatentable but high-value assets like: - Open pragmatic trial platforms: 30x cheaper than traditional trials, yet receive minimal NIH funding - Re-purposing generic drugs: 4,700+ clinically-tested compounds where no patent exists - Comparative effectiveness data: Head-to-Head trials that would reveal which drugs actually work best
Private companies cannot profitably fund these, so they are the only thing the NIH should be funding. Instead, the NIH explicitly avoids them to “not crowd out industry.” Translation: We won’t run the trials that would lower drug prices or fix problems without a patent attached.
The Committee Industrial Complex
The NIH organizational chart looks like someone tried to draw the internet:
- 27 institutes and centers
- 220+ study sections (review committees)
- 6,000+ employees
- 80,000+ grant reviewers
Each institute has divisions. Each division has branches. Each branch has sections. Each section has units. It’s bureaucratic nesting dolls all the way down.
Fun fact: There are more NIH administrators than there are researchers working on some rare diseases.
Case Study: The $1.6 Billion Long COVID Masterclass
The RECOVER Initiative - a masterpiece of inefficiency:
Budget: $1.665 billion ($1.15B + $515M in 2024) (source) Timeline: 4 years and counting Patients enrolled: ~30,000 Trials completed: Zero Cost per patient: $55,500
Meanwhile, the UK RECOVERY trial:
Budget: $20 million Timeline: 6 months Patients enrolled: 48,000 Treatments found: Multiple, including dexamethasone Cost per patient: $500
The NIH RECOVER Initiative spent 133X more per patient to achieve infinitely less (dividing by zero trials completed).
Americans Got Sicker While NIH Got Richer
“But maybe the NIH improved health in other ways!” you might say, hope flickering in your eyes.
Let’s check the scoreboard since NIH’s founding in 1887 (and massive expansion post-1970):
1970:
- Obesity rate: 13%
- Diabetes rate: 3.4%
- Life expectancy: 70.8 years
2024:
- Obesity rate: 42% (3X worse)
- Diabetes rate: 11.6% (3.4X worse)
- Life expectancy: 76.4 years (only +5.6 years, mostly from fewer people smoking)
During the NIH’s trillion-dollar spending spree, Americans got:
- Fatter
- Sicker
- More diabetic
- More depressed
- More medicated
It’s like hiring a personal trainer and gaining 100 pounds. At some point you have to wonder if they’re working for McDonald’s.
Political Funding: The Disease Popularity Contest
Which diseases get funded? Not the deadliest ones:
- Breast cancer funding: $700M/year
- Breast cancer deaths: 42,000/year
- Heart disease funding: $500M/year
- Heart disease deaths: 700,000/year
Heart disease kills 16X more people but gets less funding. Why? Pink ribbons are better at lobbying than clogged arteries.
The NIH budget is set by Congress, which means diseases compete in a popularity contest judged by people who think the immune system is a band.
Innovation Despite the NIH, Not Because of It
Major breakthroughs while NIH was busy:
- mRNA vaccines: Developed by companies, not NIH
- CRISPR: Discovered in yogurt bacteria research
- Immunotherapy: Pioneered despite medical establishment opposition
- COVID vaccines: Industry sprint while NIH planned meetings
The NIH is like that group member who shows up after the project is done to add their name.
The Efficiency Rating: Burning Life-Years
Let’s do the rigorous math on the opportunity cost.
Cost Per QALY (Quality-Adjusted Life Year)
- Standard NIH Portfolio: ~$20,000 - $100,000 per QALY (generous estimate)
- Pragmatic Platform Trials (RECOVERY model): ~$300 per QALY
- NIH pragmatic trials funding: Capped at $500K planning + $1M/year implementation. This is a tiny fraction of the $47B budget
The Multiplier: Every $1 spent on efficient pragmatic trials buys ~50x to 100x more health than a dollar spent on the current NIH mix.
Yet pragmatic trials remain severely underfunded despite the ADAPTABLE trial proving they cost 30x less than traditional RCTs ($14M vs $420M).
The “Death Equivalent” of Misallocation
When you misallocate $40 billion a year into low-efficiency buckets instead of high-efficiency buckets, you aren’t just wasting money. You are burning time.
Annual Opportunity Cost (Central Estimates): - QALYs Lost: ~100 million life-years per year - Deaths NOT Prevented: ~7 million death-equivalents per year
Conservative 90% Confidence Interval: - QALYs Lost: 10 million to 820 million per year - Deaths NOT Prevented: 0.7 million to 64 million per year
Even in the most conservative 5th-percentile scenario, NIH misallocation costs ~10 million QALYs and prevents ~700,000 deaths’ worth of health gains annually.
In the 95th-percentile scenario, it’s burning health equivalent to most of the global death toll (60M deaths/year).
The NIH isn’t just inefficient. By blocking the shift to high-efficiency trial platforms, the current budget allocation is actively destroying the equivalent of millions of lives annually compared to the optimal allocation.
Mathematical Conclusion: \[ \text{Efficiency Loss} = 1 - \frac{\text{Current QALYs gained}}{\text{Potential QALYs gained}} \approx 98\% \]
We are operating at ~2% of our potential theoretical capacity to save lives.
The Patient Disconnect: Zero Correlation with Health Outcomes
Here’s the most damning statistic of all:
Correlation between NIH funding priorities and actual disease burden: 0.07
That’s essentially random. You’d get better allocation by throwing darts at a list of diseases.
What patients want
- Treatments that work
- Access to experimental therapies
- Trials they can actually join
- Cures for their specific disease
What NIH funds
- Understanding molecular mechanisms
- Publishing papers in prestigious journals
- Building research empires
- Protecting institutional overhead
The system optimizes for everything except patient outcomes. Because patients don’t control the money. Committees do.
What Would Actually Work
- Pay for results: Cure = payment, no cure = no payment
- Funded young scientists: When their brains still work
- Published everything: Including failures (especially failures)
- Eliminated gatekeepers: Let patients vote with participation
- Automated administration: Smart contracts > committees
But that would require admitting the current system doesn’t work. And after $1.1 trillion, that’s an expensive admission.
Fun fact: The legal framework already exists for cost recovery in trials (21 CFR 312.8). You could implement efficient trials tomorrow. But that would upset the grant-writing industrial complex.
Conclusion
The NIH has built the world’s most expensive grant-writing academy. They’ve turned medical research into a creative writing competition where the prize is permission to do your actual job.
For $1.1 trillion, we got:
- Millions of papers nobody reads
- Thousands of career administrators
- Hundreds of committees
- Zero eradicated diseases
But hey, at least the committees have subcommittees. And those subcommittees have working groups. And those working groups have task forces.
It’s turtles all the way down, and none of them cure cancer.
P.S. - The NIH will likely form a committee to respond to this chapter. Estimated timeline: 2-3 years for the preliminary assessment of whether a response is needed.